How to submit a claim on Wellbytes App ?
1. Claim Submission Process:
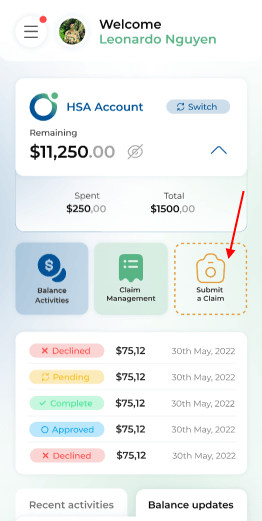
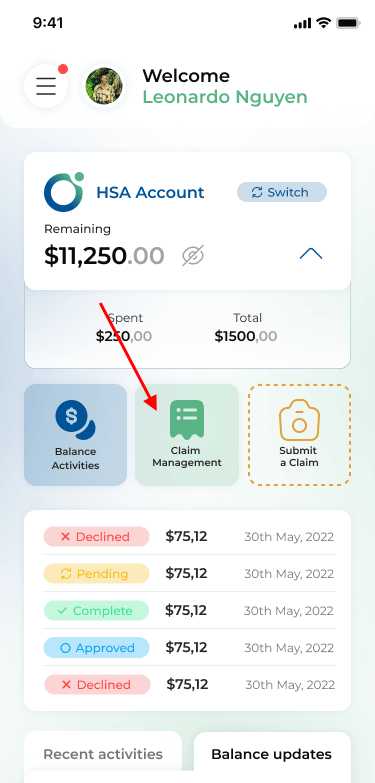
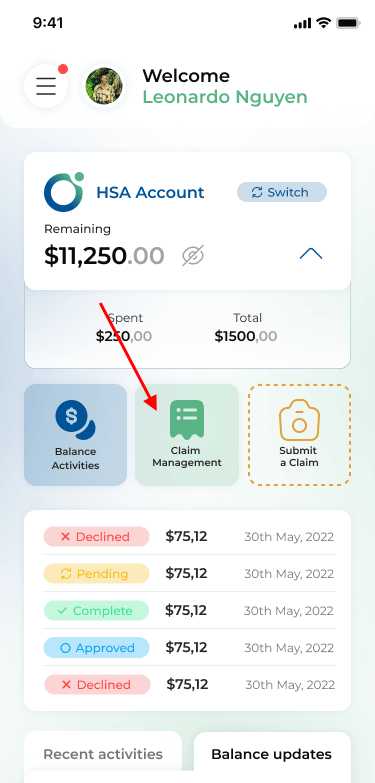
Step 1: Navigate to the main screen and tab on “Submit A Claim”.
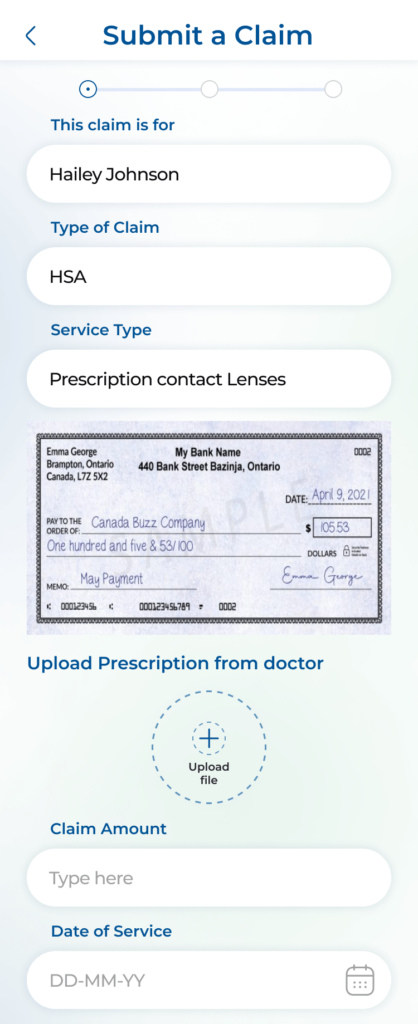
Step 2: Fill in all claim data:
- Person who is claiming (can be card holder or their dependents)
- Type of claim (WSA, HSA, Insurance)
- Service Type (type of serviced registered under the CRA that you want to submit a claim for)
- Upload required pictures of your prescription, invoices and receipts (only some services require uploading previous prescriptions from your doctor)
- Claim amount (Amount of money you want to be paid out for this claim)
- Date of service (The day you had the service you want to make a claim for)
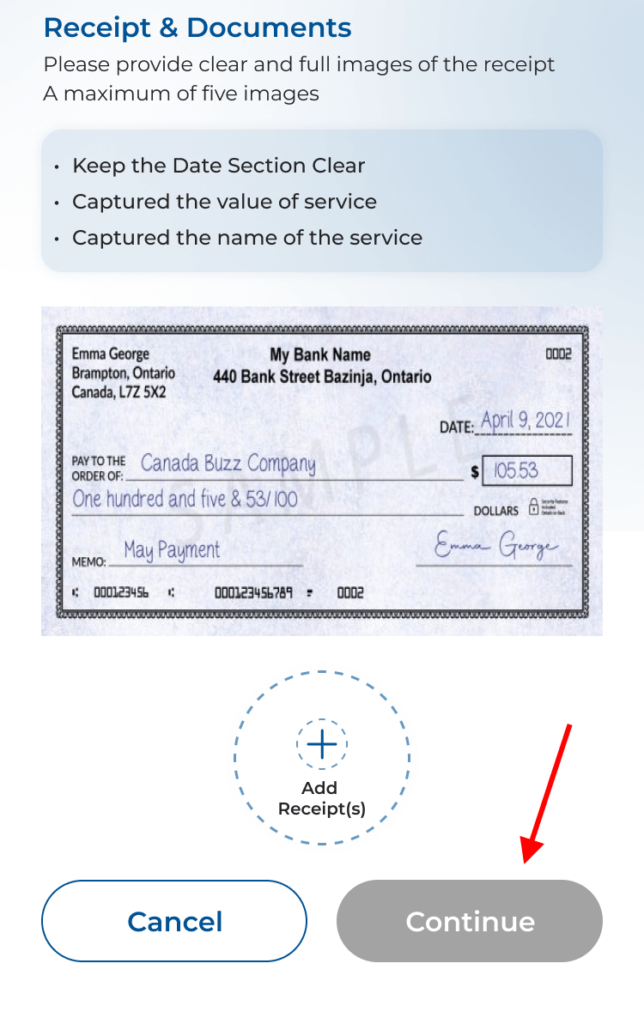
Step 3: After rechecking all the pictures are readable and no data fields have been entered correctly, select “Continue”.
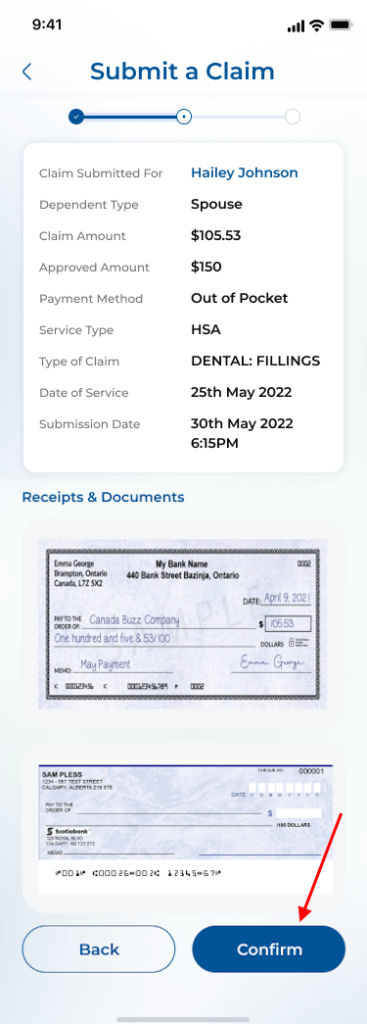
Do a final review of your claim and select “Confirm” to complete the claim submission process.
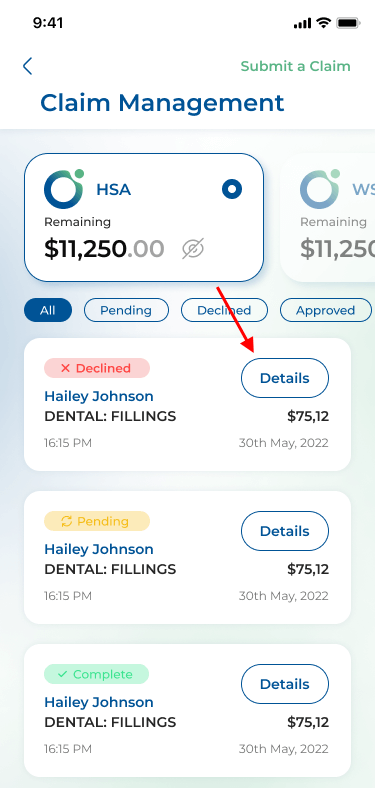
2. View Submitted Claim:
Navigate to the main screen and go to “Claim Management”.
The system selects your default viewing service and all the claims for that service will be shown.
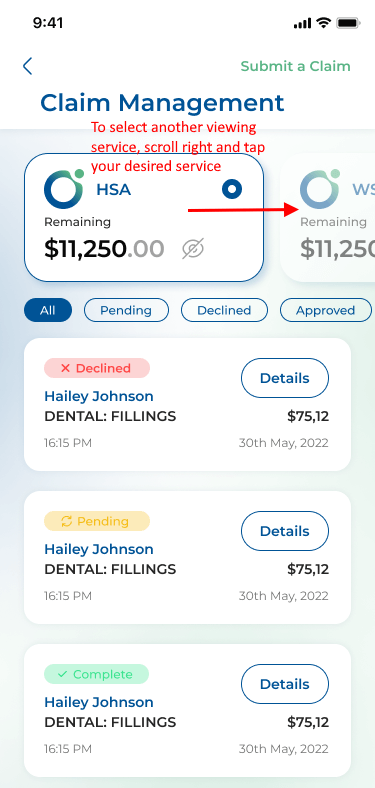
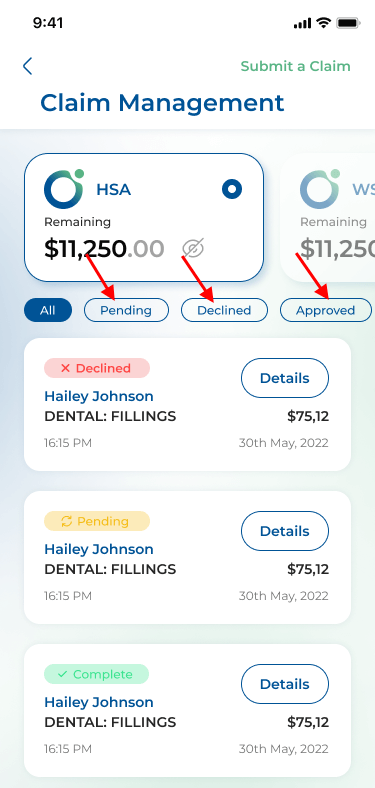
There are 4 statuses of a claim:
- Pending: the claim is successfully submitted and waiting for review.
- Declined: the claim is denied.
- Approved: the claim is approved, awaiting final bank transfer.
- Completed: the claim is approved and final bank transfer is completed.
To view only one status type, select the tab next to “All”.
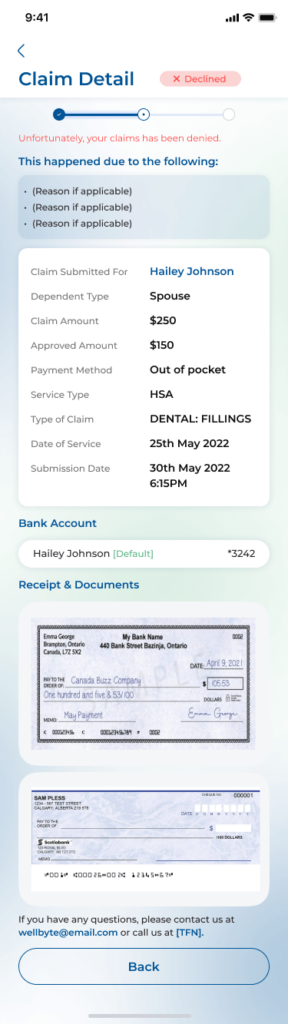
3. View Claim Detail on Wellbytes
Navigate to “Claim Management”.
Go to a claim you want to see in detail -> Select Details.
You will see a listing of all the details you have filled for that claim before. For “Declined” claims, there will be a Reason(s) tab for declining.
4. Track Claim Progress:
- After submitting a claim, will be sent a notification on phone app and confirmation email.
- Any updates regarding the states of a claim will be reported via email and phone notification channel.
Thank you for trusting Wellbytes HSA to support your health benefits journey. Our team is committed to making your experience as seamless and rewarding as possible!
